The Patient Comes First – Patient Experience
Whole-person care, integrated care, shared decision making, and patient portals have two things in common; patients and engagement. While each of the elements deserves attention, patient experience is the focus. There are many definitions of patient experience, but the following provides a compilation. Patient experience “encompasses the range of interactions that patients have with the health care system, including their care from health plans, and from doctors, nurses, and staff in hospitals, physician practices, and other health care facilities. As an integral component of health care quality, patient experience includes several aspects of health care delivery that patients value highly when they seek and receive care, such as getting timely appointments, easy access to information, and good communication with health care providers. ”
As an aside, while not specifically stated, one reality of healthcare comes through in the definition. Patient experience is one of three measures that make up the healthcare “triple aim.” It refers to a method for reducing costs by focusing on improving the patient’s experience, improving the health of populations, and reducing the cost of care. A cynic might think that patient engagement is just a method to reduce costs; I prefer to think it is a method to break down the wall between medical and individual to provide individual respect.
The change in the relationship between doctor and patient reminds me of an old joke:
“A doctor died and went to heaven. When he got to the gates, he found that there was a long line to get in. He went to the front of the line and told the angel that since he was a doctor and that doctors are important people, he should be allowed to bypass the line and go right in.
The angel replied: “Up here, everyone is equal. Now, please go to the end of the line and wait your turn.” The doctor grumbled but did what was requested. After a while, someone with a white smock and stethoscope walked right past the line and straight in. The doctor ran right back to the angel and said: “Hey, how come you let that doctor right in and not me!” The angel replied: “That’s not a doctor; that is God playing Doctor.”
When patient experience is the rule, this joke will no longer have an audience.
Shared Decision Making
One aspect of patient experience is shared decision-making (SDM). SDM is a process where patients and clinicians work together to make health decisions that follow the patient’s priorities. The value of SDM is the inherent collaboration that results in a collaborative medical decision. SDM should not require a specific level of education or economic status; it should be available to all patients without regard to these issues or any other. SDM, when applied, can help bridge any health disparities that may otherwise occur.
Substance Use
Patient experience has a unique relationship to substance use disorder treatment (SUD). Patient-centered care is a cornerstone of SUD treatment. Patient-centered care is defined as “Providing care that is respectful of, and responsive to, individual patient preferences, needs and values, and ensuring that patient values guide all clinical decisions.” Closely related to shared decision making patient-centered care facilitates patients’ access to care and commitment to care, key elements of SUD treatment.
Mental Health
Mental health treatment provides a unique challenge to patient experience. However, if we agree that patient experience is critical, it must apply to the continuum of care, including mental health care. The challenge may not be the providers but the stigma attached to the treatment. Patients may not want their information shared across all of their healthcare providers. Other issues might be the privacy requirements, involuntary commitment, and the shortage of providers. We cannot treat this as a problem unique to mental health because about one-third of people with serious medical conditions have mental health symptoms. Given the relationship between the two, for patient experience to be successful, we will need to remedy the issues unique to mental health.
Behavioral Health Home
A behavioral health home (BHH) is a model of care focused on integrating primary care and mental health services for adults with serious mental illness. Generally, BHH includes a health navigator that helps the patient access needed care. At the same time, the concept appears to support patient experience in practice; neither providers nor clients were completely satisfied.
One study looked at nine separate components of a successful BHH. The components include integrated organizational culture, population health management, standard team-based approach, integrated behavioral health staff competency, universal screening for health conditions, integrated person-centered treatment planning, social connection, and patient voice. While these are all goals of the BHH, providers had issues Providers had concerns related to cost, providing social services not regularly provided by medical professionals, and the time it took to complete person-centered treatment planning. Patients had concerns with social connection but generally accepted the remaining elements. While both providers and clients generally accepted the BHH, component-specific challenges remain to address. Once addressed, the BHH provides an example of patient experience for those living with serious mental illness.
Integrated Care
Integrated care or integrated service delivery is defined as “The management and delivery of health services so that clients receive a continuum of preventive and curative services, according to their needs over time and across different levels of the health system.” While similar to BHH, it does not require a level of mental illness for participation. Integrated care relates to whole-person care depending on the model of integration. A primary care doctor integrated with a psychiatric mental health nurse in one program to manage care. Other programs looked to reduce the cost of healthcare with integrated care, specifically with fewer emergency room visits. Like BHH, the idea is to have a single place of contact for the patient so that the experience is consistent.
What is the Linkage to Cost of Care?
In 2019 the US spent approximately $3.8 trillion on healthcare. It is not surprising that all topics related to healthcare, including patient experience, come back to cost savings. Costs include inpatient, outpatient, professionals, and pharmacy. A program in Rhode Island that focused on integrated care found that costs did not reduce, but no increase in costs occurred. As stated above, patient experience is one of three elements of the triple aim. The question is whether the element of the triple aim is equally important to reducing costs or only important if patient experience reduces cost. A fear is that patient experience may prove too much of a challenge to focus on the triple aim.
Patient Experience
Patient experience is how we interact with doctors, clinicians, laboratories, and any persons or processes related to our healthcare. Some will say that the focus on patient experience came with the introduction of the “triple aim.” I prefer to think it rose out of the individual’s desire to be acknowledged and the leader in their healthcare.
Patient experience requires that all healthcare workers acknowledge the patient as the key decision-maker. It allows the patient to base decisions on the important drivers in their life, not the fifteen minutes the provider spends with them. In a recent benchmark published by the Beryl Group, 63.8% of people surveyed indicated patient experience as a top priority for them. The respondents included hospitals and non-hospital organizations. While only one study, it does present evidence that the move to patient experience is more than the triple aim but important as an individual driver.
Outcomes
We measure outcomes to determine the value of the care provided; value is the measured improvement related to the cost of care. Notice the absence of any language related to patient experience, no measuring of the patient’s experience. Measuring outcomes by cost never address the patient’s feelings, perceptions, or experience. To commit to patient experience, our definition of outcomes has to change.
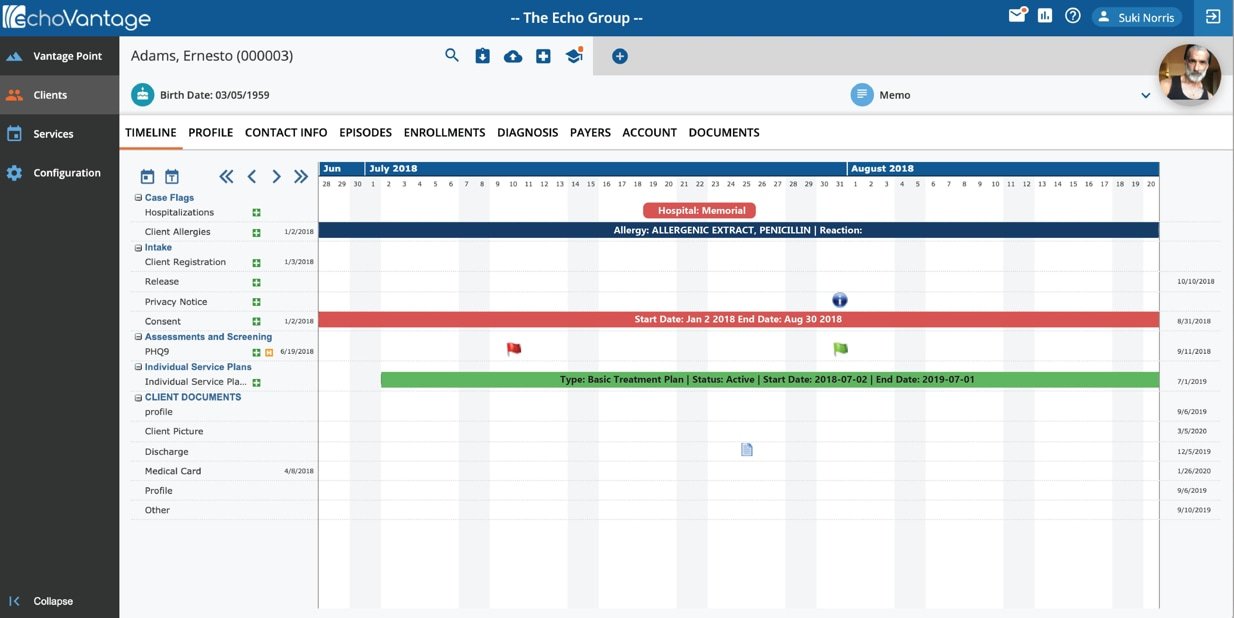
The Experience of Care and Health Outcome Survey (ECHO) is one survey that works to put the patient first. The survey designed for behavioral health looks at various measures, including access to care, receiving care without long waits, communication with clinicians, family involvement in care, perceived improvement in functioning, patient’s rights, and experience with the health plan. Notice no questions related to cost, rather focusing on the patient’s experience. It may be that patient experience went beyond the concept of outcomes to the patient’s expectations and were the expectations realized. Whichever the correct set of measures, payers require outcomes, so we must involve patients in defining the appropriate outcomes to measure patient experience.
Last Thoughts
In 2018, I presented a webinar, “Why True Integration Requires a Primary Focus.” In the webinar, I suggested that true integration starts with behavioral health and that the dollars should be in the client’s hands to make the ultimate decisions about care. Certainly one measure to develop the patient experience.` In “The state of Patient Experience 2021,” I am not sure that my proposition will work, but I do believe that patient experience is the correct direction. It has the power to make the person the center of care without regard to race, gender, sexual orientation, disability, education, or social-economic status. It makes healthcare accessible by all just as it should be.