Patient Engagement 2022 – Six Things That Will Make a Difference
In our last article, we underscored the importance of patient experience. But that was thinking about what we have learned; in this article, we look to where we go in 2022. Will the focus on the future of patient experience from educating the patient or increasing the provider’s willingness to participate? And are the solutions technology-based or based or person to person? Let’s take a look.
Increased Internet Access
We know that the future of patient experience includes digital connection not exclusively, but it is very important. Patient experience may find an assist from the recently passed infrastructure law. The law includes $65 billion to improve rural broadband and provide affordable access for lower-income households. The law includes an additional $2.75 billion to help states develop comprehensive plans to ensure equal access to the Internet for historically underserved communities. Many of the future predictions rely on access to the Internet.
1. Patient Portal
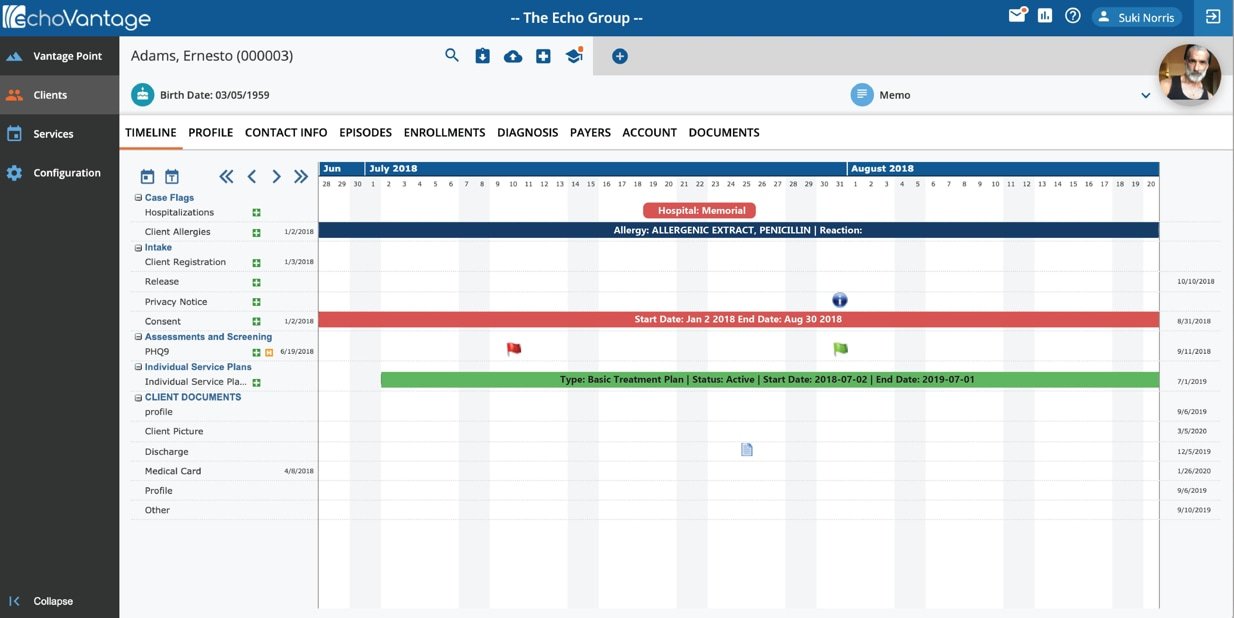
The future includes increased access to a Patient Portal that provides easy access to patients and links directly to the EHR. A patient portal is a secure online website that gives patients convenient, 24-hour access to personal health information from anywhere with an Internet connection. An effective portal connects directly to the EHR, and all data moves between the two. Patient portals represent a tool that can enhance patients’ access to their health records, but some patients remain excluded from this tool.
The challenge to engage is on both sides. Many providers do not integrate a portal with their practice, making access impossible. Many barriers exist on the patient side, including language, age, race, ethnicity, social-economic status, and patient activation. The future should provide extended access to portals by improving internet access to those facing the digital divide.
We should request community providers to increase portal acceptance. Providers can use a set of questions to find out why a patient might have reticence in accessing the portal. Questions include:
Question 1: I know how to find helpful health resources on the Internet
Question 2: I know how to use the Internet to answer my health questions
Question 3: I know what health resources are available on the Internet
Question 4: I know where to find helpful health resources on the Internet
Question 5: I know how to use the health information I find on the Internet to help me
Question 6: I have the skills I need to evaluate the health resources I find on the Internet
Question 7: I can tell high quality from low-quality health resources on the Internet
Question 8: I feel confident in using information from the Internet to make health
Users answer each question on a 5-point Likert scale. The responses will help the provider understand what is necessary to get their patients on the portal. Portal access needs provider partnership and internet access; both will be available next year.
2. Patient Appointment Reminders
How can a mental health clinic save money and reduce its no-show rate? The answer is simple, patient appointment reminders. We may all remember when the reminder was a telephone call, but text message reminders are the future (if you are not using them today.) Text messages may reduce no-shows by 25%.
Patient reminders do require that the patient has a cell phone, and while 85% of people have a smartphone, but only 43% of people 75 and older have a smartphone. In the absence of a smartphone, providers must rely on patient portal messages and phone calls even in 2022. But we should not be concerned as smartphone ownership has increased every year, so the future of text messaging for all patients may be the goal of 2025.
3. Automated Personal Outreach
How many of us have gone online to obtain healthcare information? Whatever the number is today, that number will increase in 2022. Personal outreach from the provider to the patient is more than an appointment reminder; perhaps it is a medication reminder. Or maybe it is health information or daily reminders. Personal outreach aims to engage the patient when they are not in the office.
One use is sending patient-facing survey questions to activate the patient to engage when not in the office. Measures considered include:
- Ability to self-manage illness or problems
- Ability to engage in activities that maintain functioning and reduce health declines
- Ability to be involved in treatment and diagnostic choices
- Ability to collaborate with providers
- Ability to select providers and provider organizations based on performance or quality
- Ability to navigate the healthcare system
Whether these messages come through the portal or cell phone the goal, is to maintain patient engagement.
Another program sent automated supportive text messages. Examples of the messages include, “When bad things happen we can’t control, we often focus on the things we can’t change. Focus on what you can control; what can you do to help yourself or someone else today?”
Other programs have included how tablet-based applications can reduce public health concerns such as AIDS. The public health department or providers can push information to the user’s device to encourage testing or provide reminders to stay safe.
Automated messages provide caregivers an opportunity to connect to patients to ensure safety, compliance, medication adherence, or just a nudge to promote self-management. The provider’s creativity is the only limit on the future of how we can use automated outreach to enhance patient engagement.
4. Commitment to Telehealth
We first looked at telehealth in 2020, wondering if telehealth is the future. I say yes; 2020 was just the beginning. Telehealth has proven successful across the continuum of care from treatment for COPD to providing mental health treatment to deployed soldiers. During the pandemic, behavioral health had the greatest increase in telehealth visits. Substance use telehealth has proven effective during the pandemic as well. We have learned that telehealth is effective for many services with or without a pandemic and will increase in 2022.
5. Single Shared Portal
We are moving to a truly person-centered view of healthcare. To support the view, we need to have a single share portal that provides the patient a single place to go for all health information. The idea includes primary care and specialist care in one central location. Imagine a patient who has medications from their PCP and psychiatrist, and one medication list is more helpful than going to two separate sites.
There are concerns concerning a single unified record, including privacy and provider workload. But the shared portal has provided patients’ empowerment and coordination of health care. The time has come to include the patient in the healthcare revolution and commit to the single shared porta.
6. Addressing SDOH
Health equity is part of the focus for 2022. We cannot lose focus on health equity in a world where precision medicine is the focus. In prior articles, we have talked about the SDOH from discrimination to loneliness. But know we need to look forward and understand that health equity must be part of the value equation.
As we look at person-centered care, we cannot forget the SDOH. Addressing the SDOH can reduce readmission, limit unnecessary emergency department visits, and improve poor care quality ratings. Something for everyone. By looking at the patient as a whole person, the real value is that you can address all the issues that affect health, clinical and non-clinical, and provide true person-centered care.
Final Thoughts
Charles Darwin said, “It is not the strongest of the species that survives, nor the most intelligent, but the one most responsive to change.” 2022 provides an opportunity to put 2021 in the past and focus on changes that make healthcare better for all, with a true focus on patient engagement.