What We Learned at p2p
Two years ago, we planned our annual users’ conference Peer to Peer to be in Boston. And finally, we were able to meet face to face, peer to peer in Boston. From a Red Sox game to Duck Boats, our customers from all over the country experienced Boston and learned a lot as well.
With over half of the presentations presented by our customers, attendees learned about CCHBCs, exciting ways to use Form Designer, new uses of virtual reality, and so much more.
We were excited to share our new treatment planning system, billing tricks, exciting dashboards, and our feature design methodology.
#1: New Treatment Planning System
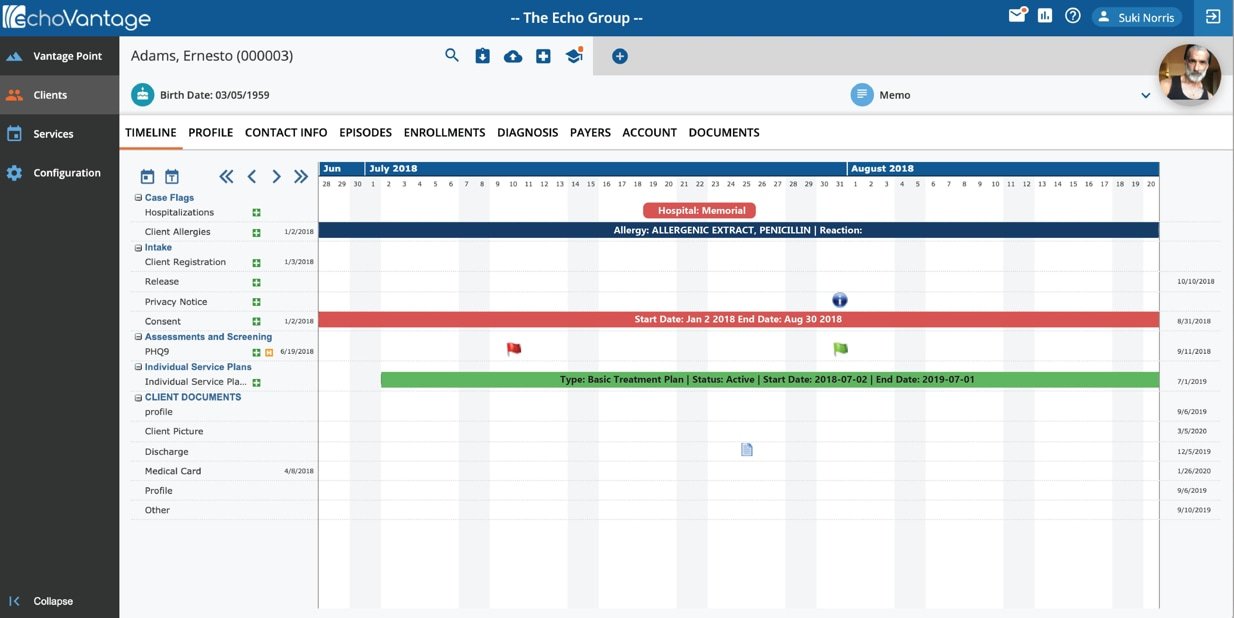
We’ve been supporting treatment plans in our EHR for the last 30 years. How the community is thinking about and approaching treatment plans is evolving. Our goal in this new feature is to provide a treatment plan that is always current. We understand that the plan must change as the client changes. New features include adding services directly from the treatment planning system. Users can also wrap all services provided during a single visit. And users can tie services directly to the treatment plan.
The new treatment planning system has increased logic as well. All details of care and progress are in a single place. Updates are automatically added to the plan, so the focus is not on updating the plan but on reviewing it. It is easy to update the plan directly from the encounter. Finally, it is a structured plan, but it supports user configuration, and there are points in the treatment planning system where you can add your own forms to collect data unique to your organization.
The underlying focus of the treatment planning system is quality. We link problems to objectives and milestones on evidence-based practices. Keeping the treatment plan front and center, users can confirm that they are addressing all issues. Users are reminded about outstanding tasks with instructions. Finally, all treatment plan versioning is automated.
The Treatment Planning System brings treatment planning into the 21st century.
#2: Collaborative Design
We provided our attendees an opportunity to select an item of new functionality, and then we engaged the attendees in a collaborative design session. The design session focused on creating a staff page using widgets so that users could select what they wanted on the page. The first step in design was selecting a persona who would use the new functionality. The persona allows us to think through the design from the user’s perspective, not ours. The persona we selected was Peppa Jackson, a clinician providing direct care. Characteristics of Peppa were that she used the product a lot, she was mildly tech savvy, a team player, and a people person. Her design imperatives included ease of use, fewer clicks, and mobile connectivity. The new functionality should be able to answer the question, “What do I need to do next.”
The next step was to collect ideas that were added to the board, like sticky notes. The focus of the collection was what are the needs the functionality should address. The audience provided various ideas and examples, including: “What to do next?”, “What’s missing for the clients in my caseload?”, “Want to see critical/priority tasks.” and “Make it easy to do the repetitive work Pippa does daily.”
Our next steps in the design process may not occur in the Sheraton Ballroom, but they will include our customers. We will review what we learned amongst our team and then regroup with customers to discuss any remaining areas of the problem and potential solutions. The commitment is not only to provide the solution but to continue with the collaborative process that began at Peer to Peer.
#3: Shalom House Art Program
Shalom House in Portland, Maine, shared information about its art program. Shalom House serves adults with severe mental illness and provides an array of community-based mental health services and a choice of quality housing that help people lead stable and fulfilling lives. The art program opened in 1994 and provides instructor-led classes and an open studio. In addition, to providing a presentation about the art program, Shalom House presented the are for sale, and there was a wonderful selection of art available for attendees to see and purchase. The same art has been presented in gallery spaces and open art festivals.
#4: Spaulding Academy & Family Services
Spaulding Academy & Family Services is a leading educational, residential, therapeutic, and foster care program, provider. Spaulding serves children and youth with neurological, emotional, behavioral, learning, or developmental challenges, including Autism Spectrum Disorder, and those who have experienced significant trauma, abuse, or neglect. The Spaulding presentation covered their use of virtual reality.
Spaulding uses virtual reality to provide experiences for students with limited mobility. Examples include swinging footage, mountain biking, skiing, and sledding on campus. Virtual reality is also used to provide emotional support, including calming or comforting experiences to implement in pre-crisis stages. Spaulding has not finished developing content; they have plans to expand virtual reality to provide support during routine medical procedures, like drawing blood. They also want to capture the content of scary places, like barbers, doctor’s offices, dentists, and courtrooms.
#5: CCBHC – The Grand Mental Health Model
Grand Mental Health provided insight into being a CCBHC. The first session discussed how they implemented access on demand, and the second session provided insight from the management team on the challenges of implementing the CCBHC. Grand discussed their use of iPads and the related reduction of emergency visits.
In 2016 Grand Mental Health introduced the GRAND model. The goals were to reduce inpatient hospitalization, build and foster better relationships with community partners, and provide a centralized location for people to seek help 24 hours a day. iPads with the GRAND model integrated support access application is distributed to GRAND clients, first responders, hospitals, and other community partners, providing instant access to a Grand therapist anytime. The program is successful, with a significant decrease in inpatient stays and a significant increase in community partners working with trained clinical staff to address crises.
Following the presentation of Grand’s success, the senior staff held a round table to discuss how the agency met the challenge of the new programs. Becoming a CCBHC requires changes to compliance, clinical services, crisis services, addiction services, staffing, operations, and finance. Grand implemented more than 25 evidence-based practices, a team-based model of care, developed services to address infant mental health, added behavioral health coaches, and moved from fee-for-service to outcome-based. While the task was great, the outcome was payment in full, and Grand reduced the number of clients who required inpatient care from 959 to 66 in six years while serving nearly three times as many clients. While implementing the CCBHC was challenging for all involved, the success provided the necessary motivation.